
What we do
A referral to the Compassionate Companion Service ensures that these essential conversations are addressed.
Equipped with time and skills and supervised by the service medical team, our companions aim to ensure that no-one faces this journey without knowing the choices available for their care. Liaison with the person’s GP completes the process so all relevant professionals can access the documentation to honour those documented choices where possible to do so.
Here are the links to jump directly to the core of our services described below:
What matters to you?
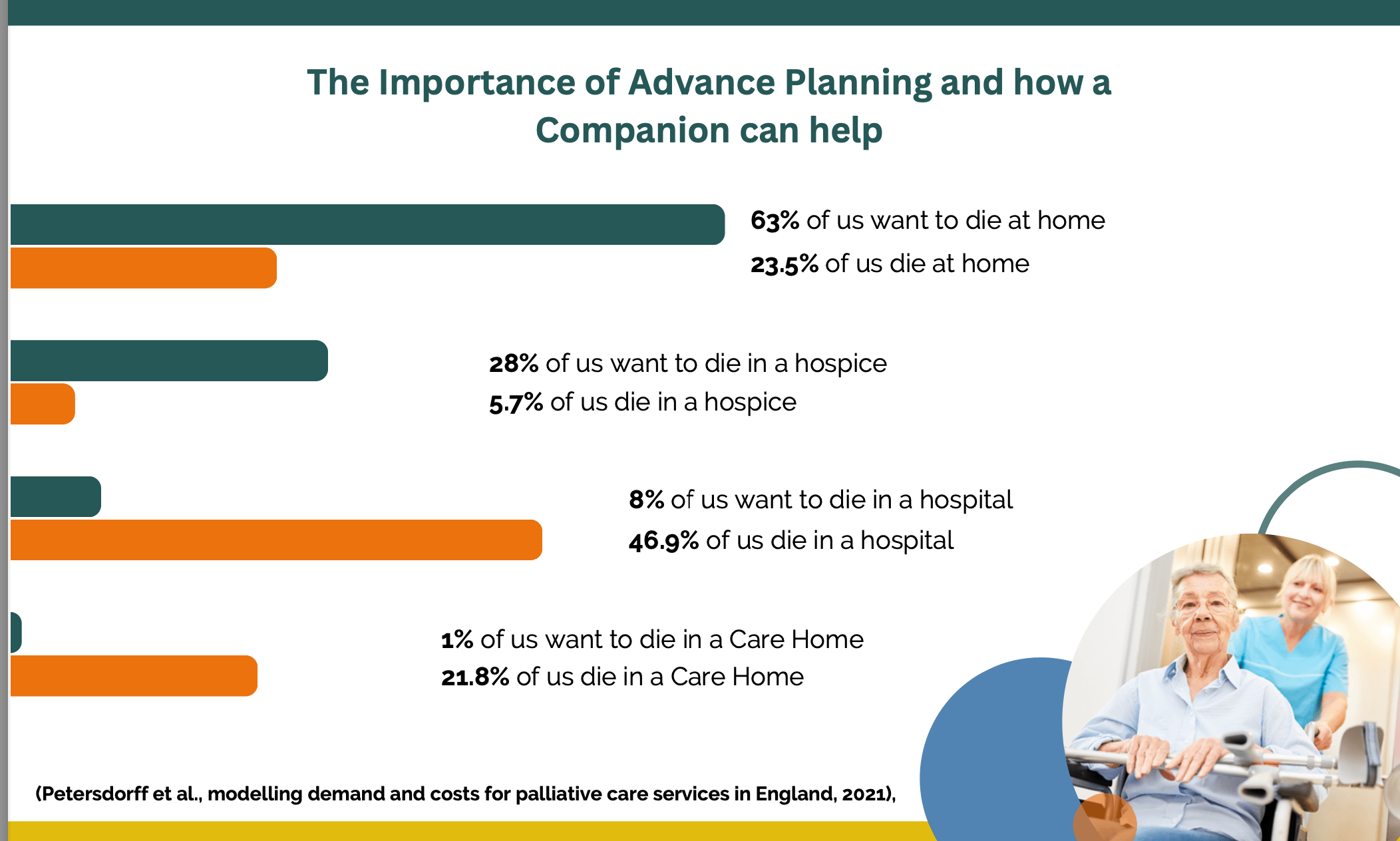
70% of us will have decisions made about our end of life care on our behalf. We all have the right to be involved in those choices yet this table illustrates that most of us are not.
Companions have the time and skills to listen, inform and enable individuals to make advance care plans that medical teams can honour where at all possible.
Improving holistic end of life care within our Communities
Learn about the Compassionate Companions initiative in Suffolk, where volunteers support those at any age with life-limiting illnesses with choice around their care.
This video highlights the importance of community involvement and open conversations around end-of-life care.
Our approach to
end of life Care
As Compassionate Companions, we understand the importance of dignity, choice, and compassion at the end of life. Using the model of the “ARC of dying well”, we support conversations about:
Advance Care Plans (A):
Our companions facilitate Advance care plans during visits with the patient. Choices around End of Life care are recorded on the ReSPECT form and these are sent to the GP for further review and sign off. Forms are then kept safely with the patient at all times.
See the link below for a helpful 10 minute film to support everyone using the ReSPECT form:
Resuscitation (R):
When the heart stops, unless stated on a ReSPECT form by an authorised senior healthcare professional, attempts will be made to restart it using cardiopulmonary resuscitation (CPR). It is a decision made by a senior clinician but essential for the individual to be involved with. Companions provide information to support understanding and facilitate discussions with their GP.
The 10-minute film below explores resuscitation more fully with patients and their families:
Care Wishes (C):
Rarely completed by healthcare professionals, care wishes include less medical but important decisions for the patient to discuss and document before/as they approach end of life.
Rather than what is the matter with you we ask “what matters to you?” – such as funeral wishes, religious/spiritual needs, digital legacy etc.
Signposting for wills and Power of Attorney, and additional care needs etc can also be done by companions.
Our aim is to ensure that each individual we support can face the end of life with their choices honoured, in comfort and with compassion.
The way we help
Support for patients
Our volunteers provide support to individuals in their final year of life, with information about the choices available to help them plan for their future care.
We aim to ensure that everyone has the chance to understand the choices available, and that once those choices are made they are recorded and shared with all involved in the individual’s care.
See our Patient leaflet to find out more about the support we offer.
Complete the Form to request a Companion (docx file)
and return it to: bill.thompson1@nhs.net

Training & support for companions
As a compassionate companion or champion our training will provide you with the skills and the confidence to support discussions about advance care planning to ensure each person has had the opportunity to make their wishes known.
Training takes place over two and a half days for volunteers, and two days for statutory workers.
Ongoing support is provided by:
- fortnightly one hour peer group meetings via Zoom for debriefing, shared learning and evaluation
- Whatsapp team group for sharing information, reflections, and comments etc
- informal ‘buddying’ between volunteers
- direct contact with the clinical lead team
- clear information regarding sign-posting when required
Fill out the Training application Form to become a Companion (docx file)
and return it to: bill.thompson1@nhs.net
Community Engagement
Through outreach and education, we work with compassionate communities to understand and support end-of-life care. This involves raising awareness, encouraging open discussions about death and dying, and providing resources to improve the quality of life for those nearing the end.

FAQs
Find answers to commonly asked questions about our services, volunteering, and support in our FAQ section below.
Volunteering
How can I become a Compassionate Companion volunteer?
Please fill out the Training application Form to become a Companion (docx file);
And return it to: bill.thompson1@nhs.net
Following your application, we’ll invite you for a chat to discuss the role in more detail and answer any questions you may have.
All volunteers are required to attend our training program to ensure they are fully prepared to support individuals in their last year of life in compassionate and non-medical ways.
What commitment is required from volunteers?
We ask our volunteers to commit to at least an hour per week to support a patient or family.
The amount of time spent with a person varies, and is mutually agreed by the companion with the individual they are supporting. In some cases this may involve weekly face-to-face contact, while in other cases there may be less regular contact, or some contact via phone.
Volunteers are asked to complete a short survey on Survey Money (easily accessible via shared link) after each contact or visit – this can be submitted anonymously, and is a requirement to fulfil the terms of NHS funding to evaluate the effectiveness of the service.
It’s essential that volunteers are reliable and consistent, as building trust and a supportive relationship is crucial to our service’s impact.
Are there any specific qualifications needed to volunteer?
No specific qualifications are required to become a Compassionate Companion volunteer. We value empathy, compassion, and the willingness to support others. Training is provided to all volunteers, equipping them with the skills needed to offer meaningful support.
Enhanced DBS checks, safeguarding and confidentiality training is provided.
Patient and Carer Support
How can Compassionate Companions support me or my loved one?
Compassionate companion volunteers have the time to listen and understand what’s important for you.There may come a time when you are unwell and cannot tell the people around you what you do and do not want to happen. By making plans now, you can document your preferences for treatment and care so your wishes are known by the right people involved in your care, and your family and friends.
Feedback from patients include:
“My family don’t have to make difficult decisions on my behalf”
“Everyone will know my choices and how best to care for me”
“I’m now surrounded by the people and the things that I love”
“My family know I don’t want my life to be prolonged when I have no quality of life”
How do I request a Compassionate Companion?
Patients, family members, or healthcare professionals can request a Compassionate Companion by filling out this Form to request a Companion (docx file)
Referral to the service is simple: if a patient is registered with a GP in Ipswich and East Suffolk, and is identified as likely to be in their last year of life, they may well benefit from support with discussions and decisions around the choices they have re their care, and plans they may wish to put in place in the months ahead, as they approach end of life.
We have an open referral system: with the individual’s consent, anyone can make the referral, including the patient themselves.
Frailty, dementia, and cancer are the top three conditions mentioned on referral forms with Motor Neurone Disease, Parkinsons disease, respiratory heart and renal failure common conditions.
Referral forms are on medical systems for primary care (dxs), community (Community care coordination centre) and acute trust referral platforms (evolve).
Once a request is received, we will work to match you with a suitable volunteer who can meet your specific needs and preferences.
What kind of training do Compassionate Companions receive?
Volunteers undergo a comprehensive training program that covers various aspects of end-of-life care, including communication skills, advance care planning, and understanding the needs of those in the last year of life. This ensures they are well-prepared to provide compassionate and effective support.
Enhanced DBS checks, safeguarding and confidentiality training are all provided.
Training
What does the training for Compassionate Companions involve?
Our training program includes a mix of theoretical knowledge and practical skills, focusing on non-medical compassionate support, communication, advance care planning, and understanding the emotional and psychological aspects of end-of-life care. Training is delivered through workshops and online resources.
Training for both volunteer companions and statutory workers involves:
- 2 days in-person training programme with Dr Crockett, the clinical team, and 2 experienced companion volunteers
- volunteers then complete a further half day of facilitated online training via Zoom that covers safeguarding and confidentiality
- Statutory workers undergo safeguarding and confidentiality training via their own organisations
Can healthcare professionals attend the training?
Yes, healthcare professionals are welcome to attend our training to enhance their understanding of compassionate care at the end of life.
Companion Champions are statutory workers in the health, care, and social service sectors who want to upskill their End of Life training to utilise within their post and during their working hours.
We have trained a wide-ranging variety of statutory worker Champions including GPs, community and hospital-based therapists, clinical Nurse Specialists, care home and domiciliary care staff, PCN patient coordinators, Integrated Neighbourhood Team staff (therapies/nursing), as well as 3rd sector employees/volunteers.
Is there a cost associated with the training?
The training is provided free of charge to both volunteers and statutory workers.
Please contact us for more details regarding training, or return your Training application Form to become a Companion (docx file) to:
